Insulin Hormone Role in PCOS

Insulin plays a significant role in the development and management of polycystic ovary syndrome (PCOS). PCOS is often associated with insulin resistance, which is a condition in which the body’s cells do not respond effectively to insulin, leading to elevated levels of insulin in the blood. Here’s how insulin is involved in PCOS:
1. Insulin Resistance in PCOS:
Insulin resistance is a common feature of PCOS, affecting a large percentage of women with the condition. It is believed to be a primary driver of many PCOS symptoms.
In individuals with insulin resistance, the body’s cells, including those in the muscles, liver, and adipose tissue (fat), have reduced sensitivity to insulin. This means that more insulin is required to transport glucose (sugar) into cells for energy.
To compensate for insulin resistance, the pancreas produces extra insulin, leading to elevated insulin levels in the bloodstream. This condition is called hyperinsulinemia.
2. Effects of Insulin on PCOS:
Elevated insulin levels can stimulate the ovaries to produce excess androgens (male hormones), particularly testosterone. This excess androgen production contributes to the hormonal imbalances seen in PCOS.
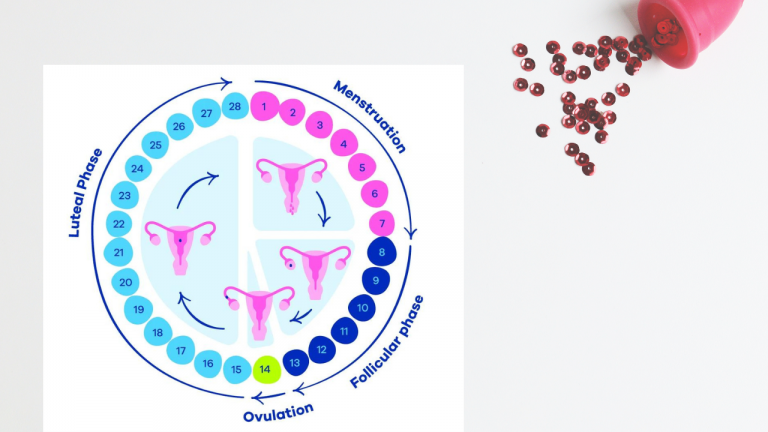
High insulin levels can also interfere with normal ovulation by disrupting the delicate hormonal signaling involved in the menstrual cycle. Irregular or absent menstrual cycles are a common symptom of PCOS.
Insulin resistance is often associated with weight gain and obesity, which can exacerbate PCOS symptoms and increase the risk of metabolic complications, such as type 2 diabetes and cardiovascular disease.
3. Management of Insulin Resistance in PCOS:
Addressing insulin resistance is an essential aspect of managing PCOS. Reducing insulin resistance can help improve hormonal balance and alleviate PCOS symptoms.
Lifestyle modifications, including a balanced diet and regular exercise, are key components of managing insulin resistance in PCOS. Weight loss, if necessary, can significantly improve insulin sensitivity.
Some medications, such as metformin, are commonly prescribed to help manage insulin resistance in PCOS. Metformin is an insulin-sensitizing medication that can improve insulin sensitivity and reduce hyperinsulinemia.
For women with PCOS who are not trying to conceive, hormonal birth control methods (such as combined oral contraceptives) can help regulate menstrual cycles and reduce androgen levels, indirectly improving insulin resistance.
It’s important to note that addressing insulin resistance can have a positive impact on multiple aspects of PCOS, including fertility, menstrual regularity, and the management of androgen-related symptoms. However, the specific treatment approach should be individualized based on a woman’s unique needs, symptoms, and health goals. Healthcare providers with expertise in PCOS can help determine the most appropriate management plan, which may include a combination of lifestyle changes and medications.